Explore how anxiety can show up in your life, work, and relationships
Read on
My Experiences with Clinical Drug Trials
Apparently the only way to slow me down at all was a serious chronic illness: I was diagnosed with Relapsing-Remitting Multiple Sclerosis on January 13, 2009. I committed to a clinical trial for what became a drug called Ocrelizumab. Resilient in the extreme I am, but this tested everything the overintellectual overachiever in me had.
And what I learned along the way.
Apparently the only way to slow me down at all was a serious chronic illness: I was diagnosed with Relapsing-Remitting Multiple Sclerosis on January 13, 2009—interestingly, also one of my brothers' birthday. I committed to a clinical trial for what became a drug called Ocrelizumab, but before that, I spent 6 months poking myself with an Avonex needle and learning to cope with side effects the first two months. Resilient in the extreme I am, but this tested everything the overintellectual overachiever in me had.
Here I am in Puerto Rico. I’m not a person to be slowed down.
I probably have had MS for about 14 years, and was diagnosed at first with RA in 2007, summer. Luckily, in Nov 2008 I hit Vertigo City, and after asking for a pain management referral, got a neurologist who dared to give me valium and meclizine for vertigo and got me a MRI. I clearly remember he called me soon after the MRIs were taken, asked me to come in, and explained that the radiologist reading the MRI had panicked and called him, saying 'You have to get her back in!'. He was pretty sanguine, but also told me, "If you were my daughter, I would tell you to take this [MRI] disk and go to the emergency room at Barrow or go to San Diego." I looked at him and basically asked, "Really?" His contention, and I believed him, was that my little podunkia county could not get the team he thought it would take together in less than several months' time, whereas Barrow had everything in one place. He let me know he didn't think it was cancer, that maybe it could be MS, but oh, "you also have a disk protruding right... there." I wasn't worried really at that time, but I knew too many things were off for me not to listen.
Long Story Short
Long story short, I drove to Phoenix the next day with my hubby-bear and proceeded to have every bit as exciting and frustrating a diagnosis process as the TV show "House" presents. I believe I had seven doctors in several specialties trying to diagnose me-- a neuroimmunologist, a neuroncologist, an infectious disease guy, a neurosurgeon, a rheumatologist, and at least two other neuros. Two wanted to biopsy my brain (AHHHH!!), and luckily my hero-MS-doc held them off while I was tested for every conceivable disease. Yes, including the rare, bizarre ones. I swear.
Hanging out with a wee friend.
In the end, after eight days in the hospital, I had one diskectomy in my neck, had given lots of blood, but went home for Xmas. I had to see them four weeks later, and two things happened-- my neurosurgeon said the neck was looking good, and my hero-MS-doc gave me my official diagnosis. Sis, hubby, and myself were there. Thus began the real drama in life.
MS has a frustrating unfolding, and many years off meds because of the long term effects of the clinical trial drug 2.5 years ago crashed with a relapse involving crutches and a wheelchair. I struggle not to make sense, but to make the best. At times, the best is actually sleeping well! But what option is better than persisting?
My Advice for Others
If I have any suggestions, it would be to not attempt this kind of ride alone. I'm beginning to understand how easy it is to care for everything but oneself, but also how, with the grace of insurance, I can find other tools to help me feel less abashed by my slow slide into a less-frenetic life. Go online. Go in person. But go find the things to make life not only bearable, but proactively possible.
Sammy is a lover of the obscure, cats, and Texas. She says, “I overthink my way into drama entirely too often. My cats, dogs, and husbear are thankfully tolerant, and I know I'm blessed to have such love around me on the wild, MS-colored life.” Check out her lighthouse in San Antonio, Texas!
Does Generalized Anxiety Disorder Go Away?
In the three years since my diagnosis, I've learned anxiety is a physiological response involving hormones. If you have GAD, hormones will hit your system in a surge. Learning the whole cycle—and appreciate the times when GAD is in remission—is an important part of living with anxiety.
In the years since my diagnosis, I've learned that anxiety is a physiological response involving hormones released in the body. If you have GAD, hormones will hit your system in a surge. They will also, however, draw back over time. Learning to feel the whole cycle—and appreciate the times when GAD is in remission—is an important part of living with anxiety. Though generalized anxiety disorder never goes away entirely, the more you understand the cycle, the better equipped you are to handle GAD symptoms.
How to Deal with Generalized Anxiety Disorder
1. Understand that anxiety will come and go throughout your life.
Anxiety is not a problem that offers any quick-fix solutions. When stressful things happen, I expect that my particular gremlin will poke his head out of the wave’s crest. Knowing what to do with him and that I’ve survived his visits before helps a lot.
2. Practice riding the anxiety wave.
I've learned the shaky feeling many people experience after a stress response or panic attack is a sign of the hormone wave receding. It's actually a good thing! We often fear the strange shaky feeling. We should be looking forward its arrival. If we understand what the shakiness means, we can enjoy that another wave is over and our strength remains from our place on the beach.
3. Listen for your symptoms.
It took me 39 years to realize that the nausea, light sensitivity, and migraines I'd been experiencing were the ways my generalized anxiety disorder expressed itself. Learning how to tune in to your symptoms will allow you to sense when anxiety is affecting you, and take actions to take care of yourself.
4. Experiment with treatment that works for you.
No approach works for everyone. Experimentation means trying to figure out what works best for you. In my case, I use medication, meditation, a moderate amount of reading and learning (I have to stop myself from overdoing it), and communication. What works for you? Share ideas in the comments section below.
5. Accept that though anxiety is part of your life, it doesn't define you.
These days, when the hormones hit, or I feel a migraine coming on, I accept it. Can the beach fight the wave? Knowing that the answer is no helps.
With treatment, you can bring your symptoms into check. But since you are predisposed to anxiety, when events happen in your life, you are more likely to have bigger anxiety responses than other people.
Here's some other reading to keep going on your journey:
Originally published Oct 29, 2017. Updated March 26, 2019.
I Was Proud of Quitting Antidepressants. Now I'm Back on Them.
This author wrote happily about how great she felt going off antidepressants…then realized she needed to go back on them.
Not the author, but the head-spinning confusion of SSRis catches the vibe.
My father, a rheumatologist, routinely prescribes drugs such as prednisone and methotrexate—he’s a believer in up-to-date medicine. Yet he’s skeptical of the fact that I have been on Celexa, a popular antidepressant and anti-anxiety medication, for 13 years. When a young relative of ours fled college two weeks into freshman year, undone by the anxiety that had plagued her all her life, he wasn’t impressed. “Why don’t they just tell her she has to stay?” he demanded. (Actually, he preceded it with “Jesus Christ!”)
The point is, even among doctors, there’s still a stigma about mental illness—and about the necessity of treating it with psychoactive drugs. The notion lingers that we all should be able to pick ourselves up by the proverbial bootstraps, that anyone who can’t hack life without a pill has a moral or character flaw. This, even though today in this country one in eight adults takes an SSRI (Prozac, Zoloft, Lexapro, Celexa) or a similar SNRI (Effexor, Cymbalta) or NDRI (Wellbutrin). The rates are almost double that for women in their forties and fifties.
Though I feel zero shame about my own reliance on SSRIs—maybe because so many of the smart, original artist types I know tend toward depression, and more than a few swear by these drugs—I worry I may have contributed to the stigma myself, with an article I wrote for this magazine nine years ago. So I’m here to set the record straight: to come clean about, well, not coming clean.
In my November 2008 piece, “Club Med,” I wrote about the backlash against SSRIs, which were then as now the most commonly used drugs to treat depression and anxiety, and the ones with the least—and least deleterious—side effects. Yet books with titles like Medication Madness and Comfortably Numb were arguing that Americans had medicated away normal emotions under the spell of evil-genius pharmaceutical marketers, that SSRIs increased the risk of suicide, and that the long-term risks of the drugs were unknown. I’d gone on a low dose of Celexa, 10milligrams, six years earlier for anxiety and insomnia and had been completely cured of both. As I wrote, “The white noise in my head vanished—poof!—and a feeling of calm came over me, the likes of which I hadn’t felt since childhood summer vacations, if ever. My anger at my husband, my annoyance about the mess of our house, my stress about public appearances, all quietly abated…. For the first time in a decade, I began to sleep deeply through the night.” I quit therapy, which no longer felt necessary; I cheerfully did a book tour I’d been fearing; I wrote a novel for the first time in years.
And then, after five years of taking Celexa, I stopped. My doctor had suggested it; with my life in a less taxing place, she said, I might not need it anymore. I respected my doctor, and I was secretly relieved to no longer “need” a drug for my head.
The withdrawal, however, was harrowing. “SSRI discontinuation syndrome” had been unheard-of when I’d started Celexa, which was initially marketed as dependence- and withdrawal-free, but by the time I went off, it was well known. A week after halving my dose to five milligrams, I woke up with what I thought was the flu: headache, dizziness, achiness, exhaustion. That lasted six weeks. I spent the next nine months tapering from five milligrams to zero.
I also adopted some classically “good” habits, practices recommended to people struggling with virtually any affliction: eating better, doing hot yoga a few times a week, returning to therapy. When I wrote the ELLE story, I’d been drugless for three months. Out of what I called “Pharma Nirvana,” I was “getting used to no longer hovering above myself watching myself live, but instead was actually living. Living and yelling and stressing, yes, and often anxious and angry and sad—but with the sadness came an awareness that I had not really experienced on the drug….Time was passing. My kids will be gone soon, I’d think, and tears would run down my face.”
If that sounds like a bit much, I can now tell you: It was. As the months passed, the old feelings and behaviors reemerged—all of them, like before, annoying and debilitating but not life-threatening—until one day, sitting in my therapist’s office alternately whining about my wonderful, chosen life and weeping because everything seemed just so sad, I begged her to affirm what I felt sure of: I was a tad, um, depressed, wasn’t I? When she agreed, I hightailed it back onto Celexa, felt worlds better soon after, and have been on it for the last seven years with no plans to ever abandon it again.
Since then, I’ve noticed that we read a lot of stories like mine, about people getting “free” of these drugs, but we rarely know what happens later. This makes sense; there’s a certain euphoria and nobility that comes with kicking a drug for the mind, something that, if you’re a writer, makes you want to, well, write about it. Two years ago, in a series of riveting essays for the New York Times called “Going Off,” Diana Spechler chronicled her decision to wean herself from a trio of psychiatric drugs because of their “grim, unbearable” side effects. The 11 columns spanned five months; by the final installment,she was “20 days med-free, eating only whole foods, stepping back into the world, a yoga mat strapped to my shoulder.”
Twenty days isn’t a long time to be off an antidepressant; some of these drugs don’t completely exit your system for weeks. I wondered: How was Spechler coping now? And then there was Patricia Pearson, the author of the gorgeous and philosophical 2008 book A Brief History of Anxiety: Yours and Mine—which I’d referenced in my earlier piece. Her book, too, was written right after she’d stopped taking first Effexor and then Lexapro, which she’d used to help her cope with quitting Effexor. It ended as she hit her six-week drug-free anniversary. But again, what happened after the six weeks…or six years?
I got my answers. But first, I want to address some of the controversy and doubt about SSRIs—a shadow that hasn’t lifted appreciably since I last wrote about this.
First, it’s true that even though it’s been 30 years since Prozac hit the market, no one knows exactly how SSRIs and their cousins work, although that’s the case with medications for everything from penicillin for infections to acetaminophen for pain relief. One long-standing theory is that SSRIs recalibrate levels of neurotransmitters—dopamine, serotonin, norepinephrine—which brings relief to people with a supposed deficiency of them.
But depression is a complicated illness, with multiple causes—some mix of genetic, environmental, and psychological components—and different symptoms for different people (anxiety, sadness, apathy, hopelessness, irritability, fatigue, change in appetite, suicidal tendencies), not to mention different side effects from its medications. Treating it is as much art as science. “Even as I faithfully took my pills,” writes Daphne Merkin in her new memoir, This Close to Happy: A Reckoning With Depression, “I couldn’t help wondering: Was I medicating a bad childhood or a chemical irregularity?”
That said, we do know that SSRIs help a lot of people, whether alleviating chronic mild depression (dysthymia) or preventing attacks of the major, paralyzing variety. Here’s Merkin again, who’s taken psychiatric drugs for more than three decades: “It’s only when I begin to sink that I remember why I am on antidepressants to begin with, which is they seem to keep me from hitting rock bottom.”
Second, it’s also true that no one is sure of the long-term impact of these drugs. Some—among them Katherine Sharpe, who wrote Coming of Age on Zoloft: How Antidepressants Cheered Us Up, Let Us Down, and Changed Who We Are—believe that “the brain habituates to SSRIs,” so that when they’re withdrawn, depressive symptoms come sneaking back. The corollary to that, of course, is that once you start, you can never stop. I asked psychiatrist Peter Kramer—who wrote the landmark Listening to Prozac in 1993 and last year returned with Ordinarily Well, which is in large measure a defense of antidepressants—what he thought of Sharpe’s assertion. “If she means that there’s a higher likelihood of depression when you come off medicine than you would’ve had if you’d never been on medicine…it’s just very hard to research that question,” he said. In Ordinarily Well, he calls a theory like Sharpe’s the “nightmare scenario” and, ultimately, deems it implausible—partly because he’s seen patients give up SSRIs and do fine, and partly because there are shortcomings in the research that supposedly proves they’re doing harm.
Even Sharpe admitted, in a piece in the Atlantic, that “SSRIs have been around for 25 years, and anecdotal reports of catastrophic ill effects have yet to emerge.” (There is something called “Prozac poop-out,” a sudden return of depressive symptoms after sustained usage. Though he hasn’t encountered this in his own practice, Kramer, a professor emeritus at Brown University, doesn’t dismiss it outright, comparing antidepressants to insulin for diabetics. “It’s not that insulin fails at its job, it’s that it doesn’t do everything,” he writes. “Something comparable may occur with antidepressants in depression; they help whatever brain system they are helping, but the underlying illness will break through, so that more or different help is needed.”)
In contrast, the risks of not treating depression are considerable. Once the illness sets in, it’s harder and harder to interrupt—and the longer someone remains depressed, the more likely the illness will continue or recur, and with more virulence. Plus, persistent depression may, among other things, cause memory loss and increase the chance of Alzheimer’s, Kramer says.
Perhaps what has stoked the biggest suspicion about the value of SSRIs are studies that suggest they work no better than placebos. To be clear, few experts make this argument with regard to treating major depression—the drugs are widely judged effective for that. The controversy focuses on the milder manifestations of the disease. In his new book, Kramer documents myriad flaws in data collection and interpretation that undercut this conclusion; for just one persuasive example, he offers evidence that a significant swath of the subjects participating in SSRI trials aren’t actually depressed, so of course they improve on “dummy pills,” as he puts it.
For my part, I’m not sure I care whether or not it’s the placebo effect that’s responsible for the transformation SSRIs have wrought in my life. I don’t believe it for a minute, but then placebos have been shown to mitigate the symptoms of all kinds of physical illnesses,after all. Mind-body dualism is dead.
It came down to this: The amount of time,energy, and money I was spending in an effort to feel half as well off Celexa as on it seemed ridiculous—notwithstanding how much I vibed with high-flown thinking about the virtues of feeling one’s feelings. “It is necessary to go / through dark and deeper dark / and not to turn,” the poet StanleyKunitz wrote. Rumi: “You are the cure for your own sorrow.” And the chronically anxious philosopher Kierkegaard theorized extensively about the condition as a source of creativity and personal growth: “Who ever has learned to be anxious the right way has learned the ultimate.” (Today, anxiety disorders are the most diagnosed mental illnesses in the U.S., though anxiety and depression often overlap and are now considered essentially flip sides of the same coin.)
pills, pills, pills, pills, pills
I get all this—and I’m also disquieted that a record number of young people take SSRIs, for longer and longer periods. Will this interfere with their ability to fully experience,and thus learn from, the glories and rigors of growing up: finding love, discovering what you want and don’t want? Curbing negative emotions isn’t always ideal for artists, either. A writer I know told me she’d tried an SSRI and felt her lifelong anxiety dissipate, but with that, she had a sudden lack of need to do the thing that had quelled it—writing—which was also how she made a living. So she gave up the drug, and the writing came back.
To be sure, there are many “cures” to try before going the medication route, as long as you’re not suffering from major depression or anxiety: therapy (psycho- or cognitive behavioral), regular exercise, even various diets. I know someone who eliminated her depression by going gluten-free. ABC anchor Dan Harris, the author of 10% Happier: How I Tamed the Voice in My Head, Reduced Stress Without Losing My Edge, and Found Self-HelpThat Actually Works—A True Story, trained himself to meditate after having a panic attack on air. And some people decide they need their dreary emotional state, at least for a while. I begged a friend who couldn’t get out of bed after the 9/11 attacks to try an SSRI, but she refused. Later, she told me she’d had “a strong visceral feeling that my depression was caused by something I could change. I suspected that taking Prozac or Celexa would allow me to manage my feelings better—lift me out of them, even—but I wanted to grapple with them and fix what needed fixing.” And she did. She left her frustrating marriage, which was painful, but is now married to a man with whom she’s much more compatible. When she feels depressed, she quits drinking for a while, which so far has worked to set her straight again.
But I have another good friend—another talented woman—who never could settle into a career. She was always insecure or dissatisfied or just plain miserable. For years, I urged her to try an SSRI, but she worried that a drug would “change” her. I try to respect this; every person’s life is her own banana peel to slip on and all that. Still, I can’t help but think that she missed the opportunity to reach her potential and live a better, brighter life. “There are people who want to be the way they are,” Kramer told me. “But there are other people who suffer emotional pain every day who think they have to live with the way they are. And they sometimes need a friend to say, you know, you think this is your fate because you’re in this state right now, but there are ways for you to feel relief, to gain perspective.”
Celexa never made me feel like I was a different person, just a more contented version of me. And it didn’t make me feel drugged or high, just less dissatisfied, easier to be around…a more patient person, mother, and wife. With the mild filter the drug put between events and my emotions, I could step back beforeI reacted—which I deeply appreciated.
I’m lucky, and this is key, that a low dose is enough to give me benefits without many side effects. The few I do have are minor. I’m woozy in the morning. I can’t drink, because more than a few sips of alcohol bring an instant headache. I am “lazier” medicated—but for me, “lazy” just means not shooting around like the Road Runner, making everyone in my orbit want to stab themselves in the face. I exercise daily, but I have no interest in the intense workouts I used to do. Maybe this is bad for my bones; I’m a tiny, thin person,and perhaps at 70, I’ll suffer some consequences from having chosen a drug and a walk (or reading a novel) over lifting weights or training for a marathon or suffering through a hot yoga class. I used to feel great after those classes, like I’d sweated out all the stress, but I remember thinking, Is spending 8 or 10 hours a week in this wildly overheated room just to be able to be at peace…is that really much better than popping a cheap, legal pill for the same or better result?
Which brings me back to Diana Spechler and Patricia Pearson, my fellow “going off” authors. How are they now?
Spechler is writing a book that stemmed from her column, so she wouldn’t say too much, but she shared this: “I didn’t go back on meds in any official capacity, though I did have a brief reunion/romance with benzos around election time.” She made other big changes, though—including moving from the East Coast to somewhere much warmer and sunnier. In other words, she made the sort of dramatic change that alters your life and can alter your depression.
Pearson was more forthcoming. At the end of her book, at six weeks without meds, she was a regular at both the gym and cognitive behavioral therapy, savoring her children and even going to church. Healthy stuff, for sure—but not, she admitted, enough to keep her med-free forever; she resumed Lexapro before the book even came out. First, it was because of anxiety over her hypothyroidism. Then, on the day of the book’s release, her father died suddenly of a heart attack. In short, her life got more stressful, as lives do, and she needed more than exercise and church to get by. The Lexapro eventually made her gain weight, however, so after another year, with her life back on track, she jettisoned it. But, she told me, “I hopped on and off a couple of times between 2008 and 2014.”
I reminded her that her convincing and sophisticated book was largely about how we’re using pills to vanquish anxiety that we might be better off living through. “I was mad at that time,” she admitted. “Mad at Effexor and mad at the pharmaceutical companies. Since then, I’ve become more moderate: When something’s of use to me, great, and when I don’t need it, fine.” She’s not taking anything now, but “if I got anxious again, to the point where I’m almost paralyzed with anxiety, then I’d have no trouble…getting a prescription for 20 milligrams of Lexapro.” She still believes that doctors and especially drug companies should be more honest about the side effects of SSRIs and the difficulty of getting off them. Other than probably Big Pharma itself, who could disagree with that?
My own biggest worry with Celexa is not what eventual damage it might cause—I’ll cross that bridge if I ever come to it—but that someday I won’t be able to get it and I’ll have to go off it cold turkey. The worry is irrational. I do still wonder on occasion, If I’d never found my wonder drug, would I somehow be more “interesting,” the person I was “meant to be”? What might I have written without Celexa? And what about the great artists who were famously depressed? If Van Gogh had been able to pop an SSRI with his morning OJ, would we have all his paintings?
Then I remember: I wrote three books taking Celexa and three not taking it, and of the latter, only two got published—because the third was so depressing no one would buy it. And while it’s true that we might not have all of Van Gogh’s paintings if he’d taken an antidepressant, I have a feeling we’d still have some—and he might not have taken his own life.
As for my young relative who left college because of anxiety, she went into therapy, started on an SSRI, and picked herself up off the floor. She returned to school the next fall and is now thriving. She’d like to eliminate the drugs—she’s had some side effects and chafes at the idea of being on them indefinitely—so she sometimes lowers her dosage (with a doctor’s help) and is learning to meditate. But in the meantime, thanks in large part to antidepressants, she’s making her way in the world, taking advantage of her rights: life, liberty, and the pursuit of happiness.
I relate.
Cathi Hanauer is the New York Times bestselling author of three acclaimed novels—“Gone,” “Sweet Ruin,” and “My Sister’s Bones”—and two essay anthologies, The Bitch in the House and The Bitch is Back, which was an NPR Best Book of 2016. She’s contributed articles, essays, and criticism to The New York Times, Elle, O, Real Simple, and many other publications, and is a co-founder of the New York Times “Modern Love” column. Find her at her site or watch her Ted Talk.
The original piece that Cathi refers to here was published in 2007 in Elle Magazine, and this piece appeared originally in Elle Magazine in 2017.
Try Throwing Some Clay to Find Some Peace
My professor likens opening the kiln doors to Christmas morning. You never know exactly what to expect but you’ll get something, even if it resembles a lump of coal.
Like most folks who come here to Beautifully Voyage, I’m a chronic overthinker. I’ve learned to compensate for the brain buzz by staying preoccupied most of my life. Until about 10 years ago, my main outlet for keeping myself busy was baking. Measuring the ingredients with a scale (like most serious bakers, I am OCD about measurements), following linear instructions, and producing something that gives pleasure quiets my brain from obsessing about, for instance, how in third grade I was waiting in line for recess and told my friend that I was going to die by the age of 45, and how I turn 45 next year, and, you know, what if that somehow comes true?
But then I transitioned my career from graphic designer (also detail obsessed) into baking and developing recipes. I founded my blog Eat the Love, then wrote a baking cookbook called Marbled, Swirled, and Layered. And I started to find that the kitchen was no longer a place for me relax; now it was a place to work. Fun and satisfying work, but work nonetheless. My former space to get out of my head was suddenly a cause of stress. I needed a new hobby.
In this age of social media, hobbies for the sake of private fulfillment are becoming a thing of the past. What used to be fun for the sake of fun has now become a public display of people who want you to know they are trying to #BeAuthentic, #LivingTheirBestLife, and #LivingTheDream. Also, Instagram and Etsy have made it possible to make hobbies into careers. That is wonderful for the few who bubble up to the top and actually make money. But it also means there’s pressure to both excel in your hobby and to make money from it. If you aren’t getting hundreds and thousands of likes on social media and money from Google Ads then why bother? There is no longer space for mediocrity and that’s unfortunate. Because sometimes, doing something for the sake of doing something is the whole point.
About three years ago, I signed up to take a continuing education class in ceramics on a whim. I thought it would be fun to make my own plates and props for my food photography. I had taken a ceramics class many years in high school and I figured it wouldn’t be too difficult to pick up again. I figured wrong. Every piece I created was garbage. But a funny thing happened as I made my clunky ceramic pieces—I fell in love with making pottery.
Here’s the thing about clay as a medium: it is both one of the easiest mediums to work with in the sculpture space as well as one of the most difficult ones. There is no other medium that allows you to immediately create a shape with minimal skill. If you want to create a dent in your piece, you just place your thumb into the clay and push. Every other medium has you carving, hammering or chipping away to get that dent. With clay, you just push and you have it. No other medium allows for this immediate result.
But unlike other mediums, the process to make that shape permanent, is fraught with potential mishaps. Drying the piece improperly can cause cracks in the clay. The dried, unfired clay (called greenware) is fragile, and be ruined if dropped or roughly handed. The clay can explode in the kiln for a number of reasons, including improper preparation of the clay, not properly drying it, or having air holes in the clay. Then, assuming you even get to the next step, glazing the piece poorly can result in in shards of glaze (which is basically glass) falling off. And if you work on the wheel throwing pots, the chances for error become exponentially larger as you try to center and pull each lump of clay into a perfectly symmetrical (good luck!) functional item. Even seasoned ceramic artists know that there is an element of surprise and magic in the outcome. Some of the best potters exploit that, creating unique pieces that are impossible to replicate. It’s a humbling experience and that’s exactly why I love it.
I’m not the only person who feels this way about ceramics. A few years ago the New York Times wrote about how ceramics was the new pilates and last year Vogue declared it the new yoga! Ceramics not only requires an attention and focus on detail but it is also a way physically be in the moment, almost a form of mediation. Nearly everyone interviewed for the article talked about it as a form a therapy, as if the clay somehow is able to absorb your stress and emotions, while those quoted in the Vogue article refer to ceramics as a “holistic antidepressant.”
I’ve spent the last three years trying to master the potter’s wheel and I’m still learning. I recently started using porcelain, a type of clay that is notorious for its exacting nature, and I feel like I’m starting at square one again. It’s challenging and rewarding work though, as throwing porcelain clay will just make me a better, more refined potter.
I imagine working with clay will be a lifelong pursuit, as every time I learn something (or think I learn something) there are five more things for me to learn or deal with. I talk to potters and ceramic artists with 15 or 20 years experience and they say the same thing--at every turn, every step, something comes up that is potentially problematic. You can invest days, weeks and even months working on a piece, only to have it fall apart in the end. But when it does turn out how you expected--or even better--it’s a wonderful feeling. My professor likens opening the kiln doors to Christmas morning. You never know exactly what to expect but you’ll get something, even if it resembles a lump of coal.
Working with clay is so absorbing for me that I can’t obsess about anything else. I can’t worry that I didn’t wash my hands after using my iPhone and then ate a handful of potato chips, which will surely give me a severe foodborne illness, because in my mind the iPhone is one of the dirtiest surfaces on the planet. I can’t fret that I inadvertently insulted a friend because I still haven’t written about her cookbook on my blog even though she totally wrote about my cookbook on her blog. All I can do is concentrate on the clay in my hands, especially when I use the wheel. I concentrate on wedging the clay, centering it, creating a hole in the middle then pulling the clay up into a cylinder; that’s it, but that’s everything. Any time my thoughts waver, the clay wavers too, so it takes all my concentration. And since my hands are dirty with wet mud, if the phone vibrates I have to make a choice between getting up and to wash and dirty my hands, or continue what I’m doing. I rarely choose to get up. For the entire period of my three-hour class I am usually unreachable and completely focused on the process. It’s a glorious thing.
But the biggest learning experience in clay is that sometimes (ok, often) the end result isn’t quite what you expect it to be. So instead of making that the most important part, I focus on the joy of the process and get lost in that, which many would argue is a good rule for how to approach life in general. That’s what I’m trying to do.
But it’s hard. Up until this point, I’ve avoided selling my work and turning my hobby into something that creates money. I don’t want the pressure! But I also have so much pottery in my house, it’s getting a bit ridiculous. So I’ve started up an Instagram account dedicated to my pottery, but I know it’s risky. I can feel the old allure with each like and each follower I get. I’m trying to hold on to my love of clay and working without distraction in the studio. I don’t want to be the guy that has to check his Instagram posts every 15 minutes. I’ve been down that road before and I never want to go back.
For now, I’m just going to enjoy the soothing feelings of the mud slipping through my fingers on the wheel and remind myself I have plenty of time to figure out the rest. Right?
About the Author
You can follow Irvin’s ceramic adventures on his Instagram account or follow him on his main Instagram account or his food blog Eat the Love to see his ceramics pieces in use.
How Mental Health Benefits Work for Top Bay Area Insurance Plans
Navigating health insurance benefits can be a bewildering, frustrating experience in the best of circumstances. And when you’re dealing with a mental health issue, bureaucracy and paperwork can feel overwhelming….This post can help!
Navigating health insurance benefits can be a bewildering, frustrating experience in the best of circumstances. And when you’re dealing with a mental health issue, bureaucracy and paperwork can feel overwhelming. Figuring out your mental health benefits is crucial for people in crisis (or even in everyday life). We wanted to help, so we tried to do that research for you. We’re testing whether an article like this can actually help people in the Bay Area. Please let us know if this information helped you, so we can figure out whether to do more in the series.
For this guide, we researched and dug into the mental health benefits for the top eight insurance carriers in San Francisco. We looked at top tier and lower tier plans, trying to understand what you can expect in terms of insurance coverage for mental health. If you’ve had an experience with insurance and mental health coverage or therapy, please let us know in the comments below. We want this information to be hands-on and useful.
Mental Health Benefits for Blue Shield of California
Blue Shield is one of the biggest providers of insurance in the Bay Area. If you’re working for a Bay Area-based company that provides health insurance, you were likely offered one of Blue Shield’s numerous plans, each of which has varying coverage.
If you’re a Blue Shield subscriber, the price you’ll pay differs depending on the plan you’re on. We focused on Blue Shield’s lowest tier (HMO) and the highest tier (PPO).
How Much You Can Expect to Pay for Mental Health Care on Blue Shield
If you’re on the lowest tier HMO: The Silver 70 Off Exchange Trio HMO…
If you’re on this Blue Shield plan, you can expect to get as many visits covered as you need, but you may need to ask your mental health provider to submit a treatment plan if requested. You will pay $40 copay per office visit with a mental health provider within network (more on that below). Other mental health services such as psychological testing and hospitalization will cost you 20% of total cost with coinsurance. No mental health coverage is offered for out of network providers.
If you’re on the highest tier PPO: The Platinum 90 PPO…
If you’re on this Blue Shield plan, you can expect to getas many visits covered as you need, but you may need to ask your mental health provider to submit a treatment plan if requested. You will pay $15 copay per office visit with a mental health provider within network (more on that below). Other mental health services such as psychological testing and hospitalization will cost you 10% of total cost with coinsurance. No mental health coverage is offered for out of network providers.
Here’s a link to more detailed information about Blue Shield of California’s plans to find your own price points.
What Mental Health Benefits on Blue Shield Really Look Like
Blue Shield uses a third party administrator, Mental Health Services Administrator (MHSA), for mental health benefits. With more than 2,000 providers to choose from, they hope you will be able to find help near you. Here’s what the actual experience of searching for a mental health provider looks like:
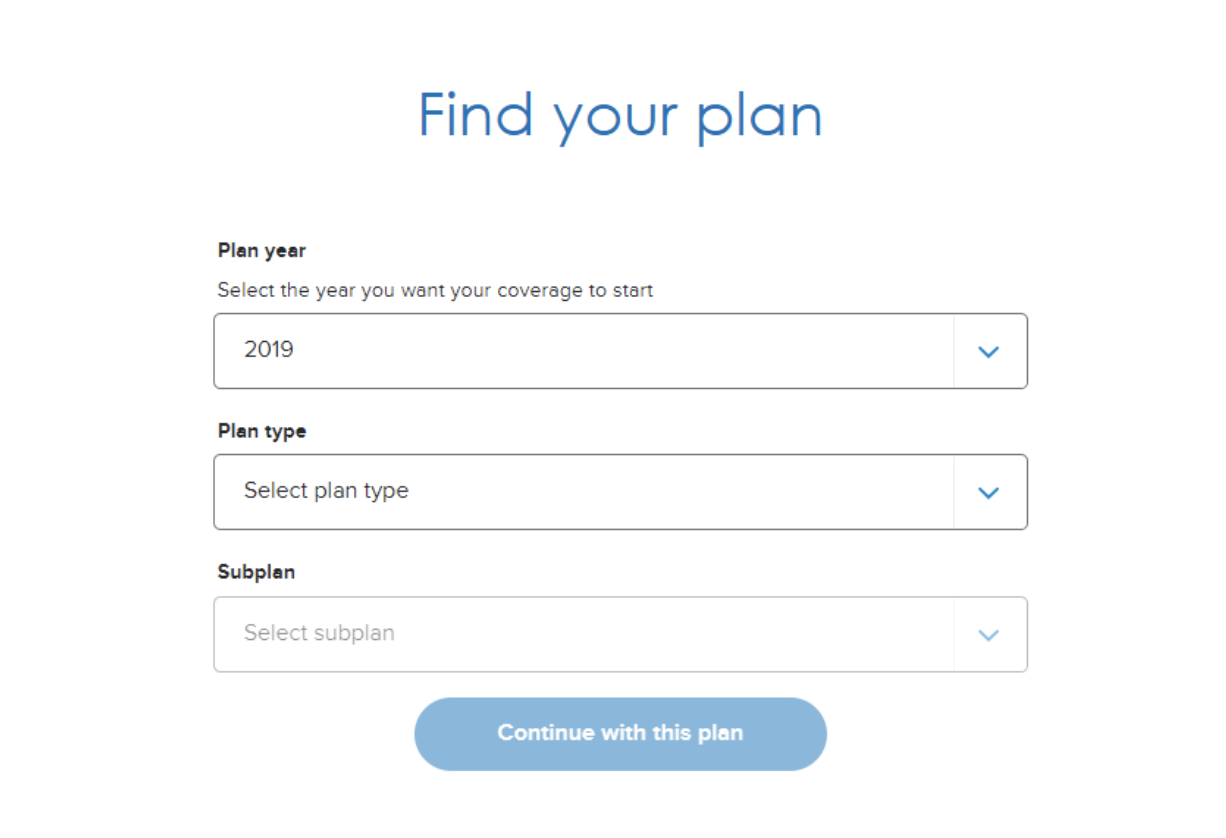
You start on on their site.
Then, when you actually try to search, you are popped into another site, which though it is described as Mental Health Service Providers, first asks whether you are a member. If yes, you’ll need to log in to access the provider directory. If no, you can search by location and plan type.
Once you enter your plan type, you’ll be taken to this screen where you’ll once again need to enter your plan type and location and choose Medicare or non-Medicare providers.
You’ll then be able to view a list of providers who fit the parameters you entered. The process is cumbersome, but in the end, you’ll receive a good list including provider contact information, provider mental health specialties and whether or not the providers are accepting new patients.
2. Mental Health Benefits for Kaiser Permanente
Kaiser Permanente has several plans with varying mental health coverage. Below, you’ll find information on their standard HMO plan. You can click here for additional information on plans and coverage.
How Much You Can Expect to Pay for Mental Health Care on Kaiser Permanente
If you’re on the Highest Tier HMO: Platinum 90 HMO…
For any outpatient mental health services, such as therapy or psychiatry visits, you’ll be charged a $15 copay per visit. For inpatient services, you’ll be charged a $250 copay per day for up to 5 days after which there is no additional charge.
The plan charges $7 per visit for mental and behavioral health group therapy in an outpatient setting.
If you are covered under the Community Health Care Program, there are no copayments for most covered services at Kaiser Permanente’s medical offices and hospitals.
What Mental Health Benefits on Kaiser Permanente Really Look Like
The Kaiser network includes 70 mental health providers in San Francisco and more than 1,200 providers in the bay area. If you choose a provider who is not in-network, you’ll need to pay out of pocket as no coverage is provided.
Here’s a look at what you can expect when you search for a provider on their provider website:
From here, you can search by specialty, location, and even gender. Tip: enter psychiatry in the specialty box for the most comprehensive results.
3. Mental Health Benefits for United Health Care (UHC)
UHC has several different plans and coverage varies. Below, you’ll find information on the lowest and highest tier plans. You can click here for additional information on plans and coverage.
How Much You Can Expect to Pay for Mental Health Care on United Health Care (UHC)
If you’re on the highest tier PPO: Select Plus PPO Platinum…
For outpatient mental health visits, the plan charges a $10 copay per office visit and the deductible does not apply. All other outpatient mental health services and inpatient mental health care requires 10% coinsurance and again the deductible does not apply.
If you’re on the lowest tier PPO: EPO Silver…
For outpatient mental health coverage, the plan charges a $45 copay per office visit and the deductible does not apply. All other outpatient mental health services and inpatient mental health care requires 40% coinsurance after the deductible has been met.
For any plan, if you choose to receive care from an out-of-network mental health provider, the plan charges 50% co-insurance for all mental health care after the medical deductible has been met.
What Mental Health Benefits on United Health Care (UHC) Really Look Like
UHC has over 1,000 mental health providers in San Francisco and the surrounding area. To find specific providers, simply click here and you’ll be taken to this screen:
You’ll then be asked to narrow your search to a specific mental health issue. You’re able to choose as many options as you need, and you can narrow your search by location and distance as well.
Once you’ve set your search criteria, you’ll see a list organized by distance from the location you entered. You can filter the list further by coverage/ plan type, license type, treatment options, availability, gender, languages, and board certification(s).
4. Mental Health Benefits for Cigna
How Much You Can Expect to Pay for Mental Health Care on Cigna
Cigna also has a wide variety of plans with differing levels of mental health coverage. For most plans, you will be charged coinsurance ranging from 20-50% for mental health services, both outpatient and inpatient and a deductible applies.
What Mental Health Benefits on Cigna Really Look Like
Cigna has an easy to use behavioral health directory where you can access a list of in-network providers in a variety of mental health sub-specialties.
You’ll first be taken to this screen:
You’ll then be able to view a list of providers matching your search criteria. You can also download a pdf copy of the list for your reference.
5. Healthy San Francisco
Healthy San Francisco is operated by the San Francisco Department of Public Health and available for those who cannot obtain health insurance. To be eligible for this insurance, you are:
Living on a combined family income at or below 500% of the Federal Poverty Level. Find out if you meet the income requirements.
A San Francisco resident who can provide proof of San Francisco residency*;
Uninsured for at least 90 days**;
Not eligible for public insurance programs such as Medi-Cal or Medicare
Age 18 or over
Participants may be treated for confidential mental health services, such as individual counseling for depression, anxiety, panic, or help with other emotional problems.
How Much You Can Expect to Pay for Mental Health Care on Healthy San Francisco
The cost for these services is determined by California’s Uniform Method of Determining Ability to Pay (UMDAP) and is based on household income and number of people in a household. More information about fees can be found here.
What Mental Health Benefits on Healthy San Francisco Really Looks Like
Click here to access their Participant Handbook.
To find a mental health provider, facility, or service, start with this page:
Then, select the service you need from the available tabs. By clicking on the Mental Health Services tab, you’ll be taken to a provider list which includes provider name, licensure, program name, contact information, and website.
6. San Francisco Health Plan
The San Francisco Health Plan provides low-cost healthcare to those who qualify. The amount you’d pay on this plan depends on your monthly income. If you are a San Francisco Health Plan member, you are eligible for mild to moderate mental health issues at no cost through Beacon Health Strategies.
You do not need pre-approval for mental health services if you are a member, but you will need to register with Beacon and go through a brief screening to receive therapy services. The therapist must be part of the Beacon network. There is no limit to the number of visits for any mental health service as long as they are medically necessary. (This is determined by Beacon in collaboration with your mental health care providers.)
Services provided include:
Individual and group mental health evaluation and treatment (psychotherapy)
Psychological testing
Psychiatric consultation
Mental health and alcohol use screening and counseling
What Mental Health Benefits on Healthy San Francisco Really Look Like
More detailed information on specific coverage can be found in this document and the plan also provides a comprehensive reference guide.
San Francisco Health Plan uses the same provider directory as Healthy San Francisco, so you’ll start at this page:
Then, select the service you need from the available tabs. By clicking on the Mental Health Services tab, you’ll be taken to a provider list which includes provider name, licensure, program name, contact information, and website.
7. Chinese Community Health Plan (CCHP)
CCHP offers numerous plans with varying coverage for individuals and businesses in San Francisco and northern San Mateo counties. Below, you’ll find information on the lowest and highest tier HMOs. You can click here for additional information on plans and coverage.
How Much You Can Expect to Pay for Mental Health Care on Chinese Community Health Plan
For all plans, the number of mental health visits per year is not specifically limited; it is based on what is medically necessary, which is determined by your primary care doctor and mental health providers treatment plan. In other words, the plan will cover the care you need based on your condition and treatment needs.
If you’re on the highest tier HMO: Ruby 10 HMO Platinum…
For outpatient services, the plan charges a $10 copay per visit. For inpatient services, you’ll be charged a $150 copay per day for up to 5 days.
If you’re on the lowest tier HMO: Opal 50 HMO Silver
For outpatient services, there is no charge for office visits; however, they do not apply to the plan deductible. You’ll be charged $50 per visit for all other services. For inpatient services, you’ll be charged a $250 copay per day for up to 5 days.
What Mental Health Benefits on Chinese Community Health Really Look Like
The provider network for mental health is comparatively small, with under 100 providers in the bay area. Out of network providers are not covered by the plan.
First, you’ll see this screen where you can search by plan type or specific doctor, facility or specialty:
Once you’ve made your selection, you’ll see an easily-navigable list of providers and facilities including location and specific CCHP plans accepted.
8. Health Net
Health Net also offers several plans. Following is a brief summary of the top tier plan (no deductible) and the highest deductible plan. Out of network providers are not covered for any plan. Be sure to check on pre-certification for all services, or you could be charged a $250 penalty.
How Much You Can Expect to Pay for Mental Health Care on Health Net
If you’re on the highest tier PPO: Platinum 90 PureCare One…
For outpatient care, there is no charge to see a preferred provider. For inpatient care, the plan requires you to pay 10% coinsurance.
If you’re on the lowest Tier PPO: Minimum Coverage PureCare One…
For outpatient office visits, there is a 0% coinsurance deductible which is waived for the first three visits. For care other than office visits, there is 0% coinsurance after the deductible has been met. For inpatient care, there is 0% coinsurance after the deductible has been met.
What Mental Health Care on Health Net Really Looks Like
Health Net has 822 providers located within five miles of downtown San Francisco. For more information on providers click here.
You’ll be taken to this screen:
After entering your search criteria, you’ll see this menu:
Click on Ancillary Services to search for mental and behavioral health providers or Doctors if you have a specific provider in mind. From there, you’ll need to enter your plan type and specific plan:
You’ll then see a list of in-network mental health for your plan which you can view in list or map view. It is also possible to export, print, save or email your results.
Conclusion
Understanding and using your mental health benefits can be a confusing process, but many plans now have resources specifically devoted to helping navigate mental health benefits. With a little research and help, you can get the help you need to care for your body and mind.
*The information was gathered in 2019 and is subject to change at any time. It’s intended to serve as a guide to help users navigate options within the mental health coverage they have. If you experience something different with one of these providers, please comment! We would love to keep this up-to-date and useful for all.*
About the Researcher
Lorna Rogahn is a medically-minded mom and wife who is passionate about mental health, medical research, parenting, and all things literary.
When not rearranging letters and punctuation on a computer screen, she spends her time chasing her speedy son and her even speedier greyhound.
How I Took Control of My Chronic Migraines
It was my birthday, my 28th birthday to be exact. I wore a bright red dress. If you looked at me, you wouldn’t have known that anything was wrong. As I waited for my six guests, I had only one thought: how can I get through the next three hours without vomiting and passing out?
I found a solution that worked for me.
It was my birthday, my 28th birthday to be exact. I wore a bright red dress because once I commit to an unnecessary idea (going somewhere fancy for my birthday so I can dress up) I go all the way. If you looked at me, you wouldn’t have known that anything was wrong. I walked briskly, impatiently and slightly in agony through the CBD towards the French restaurant hidden in a laneway. I would be the first to arrive in a small, intimate booth and I would wait there with the face of Monica Bellucci in Malena as she whips out a cigarette and all the men rush to light it, but instead of a cigarette, I’m about to pop the painkillers and they’re passing me water.
As I waited for my six guests, I had only one thought: how can I get through the next three hours without vomiting and passing out?
Hi my name is Sheree and I’ve had migraines for a decade and chronic migraines for two years. I survived my own birthday by falling into a fugue state and living through an alternate reality where I was actually a French countess or something. I gritted my teeth, I employed the occasional head in hand maneuver, complete with one eye closed during the main course, and periodically holding a cold martini to my head. I can do this, I can get through this beautiful dinner. I won’t let these friends down.
Before I knew it, it was over. Relief flooded through me. I’d be home soon. OR WOULD I? *dramatic music*
People who couldn’t make the dinner desperately wanted to meet us for drinks. My heart fell to my gut--now the epicenter of all things nausea-related. I knew that I couldn’t go, but also that I had to go. I felt myself being pulled into opposite directions like a piece of kneaded playdoh that quickly rips in two. The sentient piece continued in the direction of a bar full of corporate suits.
I followed everyone with great difficulty, eyes closed, feeling my way down grimy George Street (Editor's note: Sheree is Australian, and she is writing about Sydney). I immediately proceeded to hide in the corner, clutching my head. One of my friends, who hadn’t been at the dinner and didn’t know I had a migraine, walked past and offered to buy me a birthday drink. I openly flinched at the idea, regretting previous martinis back when I believed I had no choice but to drink and was putting the cold ones on my head. I said no a little too loudly. He laughed unperturbed and jived off towards the bar. Everyone was having a good time, except for crouching tiger, hidden migraine standing in the corner like a loser.
My best friend Sophie, like a good best friend is wont to do, pulled me aside to ask if I was okay. I said I wasn’t and I just wasn’t sure what else to do. The migraines were increasingly beginning on Fridays and would last for an entire weekend, meaning I had already become an anti-social shut-in and just coming out at all was a small miracle (the “weekend migraine” is definitely a thing). Most of all, I felt sad that I would look back on what should have been a delightful memory and instead cringe endlessly (it’s true I’m doing that right now).
And then Sophie said some words that changed how I looked at my condition.
“You have a chronic health problem, you’re allowed to take time out to figure out how to deal with it in a way that works best for you.”
It was the first time I’d heard someone call it a chronic health problem, even though it’s something that I’ve suffered with for a decade. When you hear the words “chronic health problem” you think of people who are forced to live with serious, life-threatening illnesses, bedridden or chained to their homes. You think of something constant and enduring. But actually chronic health pain can come in all forms, and many people can be highly functional in the face of great pain. It is a constant hum you stop hearing, but something that can so casually run an endurance marathon across your life.
It’s true that when my migraines went from being occasional to frequent, they changed who I was in a fundamental way. I became reclusive and struggled with basic attempts at socialising. I lost my confidence. I struggled with basic stressful situations at work and constantly dealt with the dilemma of taking a day off when I’m the sole person to run my website. My appearance changed drastically thanks to dangerous drugs that didn’t work and which when mentioned to experts, openly flinched at the idea of taking them for migraine prevention. Most of all I developed a debilitating and constant anxiety that an attack was always imminent.
But perhaps the worst part of the ordeal was discovering the stigma associated with migraine, particularly for women. I hadn’t noticed it as much before because I was less vocal about my condition. But speaking up led to hearing other similar stories and realizing I was so far from being alone in this. It also led to the most frustrating thing you can experience with this condition — everyone migraine-splaining your condition back to you with a series of “solutions” because they had a headache “that one time in their life” and found relief with X strategy that they assume you don’t know about and are willingly avoiding for some reason.
Research into why particular people suffer particular strands of migraine is limited. Although they might know how it works, they don’t necessarily know why and how to deal with them long term. As a result, a lot of treatments are trial and error. You’re usually given ways to deal with the pain and the end result, rather than prevent them for the long term. Even less is known when it comes to migraine affecting women, even though women are more prone to suffering from migraine than men.
"It also led to the most frustrating thing you can experience with this condition—everyone migraine-splaining your condition back to you with a series of 'solutions' because they once had a headache and found relief with some strategy they assume you don’t know about and are willingly avoiding for some reason."
Generally, nobody wants to wade into murky, unanswerable areas, so they stick with tried and tested methods and what they do know, which is often limited depending on their profession and field of interest.
The problem and main barrier is that few people and few doctors take the condition seriously. And why would they? Unless you’ve suffered from migraines, it’s probably hard to imagine how bad they can get. “Just a headache” is something GPs commonly say before prescribing you some, erm, Panadol. They may as well just hand out candy because I love candy and that would at least brighten my mood.
Now, full disclaimer: a lot of this is based on my personal observations as someone who has experienced this ordeal for a long time and from what I’ve learnt along the way. But the more research I did myself, the more I discovered there was a whole wealth of knowledge on this issue I had never read before, because I didn’t know to look for it.
This is because I had never heard about headache specialists until this year.
If headache doctors — board-certified headache specialists — is a new concept to you, well there’s a good reason for it. Most migraine sufferers have only ever seen a GP or a neurologist or maybe a gynecologist. The huge issue here is that many doctors have studied migraine so little and this is how they can further perpetuate the migraine stigma and trivialize the disease. And headache doctors actually experience the same migraine stigma that patients experience.
This is the stigma checklist for those playing at home:
Have you ever felt misunderstood because of your migraines?
Have you ever been told to “take an Advil” to get through the work day?
Or made to feel guilty for canceling plans because of illness?
The physicians who dedicate their careers to migraine and headache disorders spend years studying migraine disease and work exclusively with headache patients. As the article explains,
“Neurologists, doctors who specialize in the brain and nervous system, are often not well-versed in migraine, either. On average, doctors only receive four hours of instruction about all headache disorders in undergraduate education. That is not nearly enough.”
“It is no wonder so many patients leave doctors’ offices feeling confused or bogged down by misinformation. Managing migraine disease is tricky. It involves looking at multiple areas of a person’s life, including genetic history, lifestyle choices, diet and sleep habits, and exercise patterns. Without training and education, the patient-physician partnership cannot do what is needed to manage migraines.
This lack of education can also add to some of the migraine stigmas that both patients and headache doctors feel at the hands of other professionals. Some doctors see migraine as something of a mystery, making them less-inclined (and less able) to tackle the problem. That’s just one reason being an advocate for your own migraine care is so essential.
Headache specialists understand that migraine disease is a genetic, neurological condition affecting all areas of a person’s life. Other doctors, however, may not. Dr. Dodick explains the situation this way:
“Healthcare providers have gone into the profession to help people, and they want to help people. But if you are not trained in the disorder that the patients come in to see you for, you feel unequipped to manage that person. Plus add to that the historical stigma attached to migraine and those who suffer, and it’s a double whammy.”
So with all this in mind, how do you go about finding a treatment that works for you? In the second part I explain how I turned things around and eventually got the migraines under control.
Why does it take so long to heal chronic migraines? For a while, you put up with it because you don’t really think you have options. Or you have too many options and it’s overwhelming. Most of the time you’ve tried “everything” and by everything, I mean most conventional medicine that people assume includes everything. Still, nothing works.
Another common part of chronic migraine sufferers is the one least talked about: mental health and the struggle with depression and anxiety. The relentlessness of constantly feeling sick in an invisible way. Being unable to do most activities and how it gradually wears you down. How you become convinced that nothing could hurt more than this and so death doesn’t seem so bad in comparison. Headache specialists can tell you stories of patients breaking down during a session because no one has ever really listened to them before or believed their story and now they finally have hope that things might get better.
How to get closer to relief and healing
At the worst point I was having migraines every day. I was also battling withdrawal symptoms after coming off amitriptyline for migraine prevention. The combination of battling both was one of the worst things I’ve ever experienced. I knew something had to drastically change. So I took to the internet. I did my research. I spent a lot of time on r/migraine. I subscribed to everything. I spoke to people who had actually experienced chronic migraines and ignored everyone who still thought a migraine was a bit of a headache and the people who asked you if you’ve drunk enough water, or have you tried being less stressed?
I eventually found migraine apps, websites and communities who tend to focus on “pals” and “buddies” because if there’s anything us migraine sufferers need, it’s more friends (true). An example of one such community is Migraine Pal which was founded by a charming chap called Carl. I am extremely grateful for the migraine themed friendship that Carl brought to my life during some of my worst moments. The community consists of “informed migraine patients looking for medically referenced facts, better results and support from like minded people”. It’s how I discovered that headache specialists are a thing. They do great, useful lists like 14 things you should never say to someone with migraine or this list of over 100 effective natural treatment options (let’s hear it for the King of them all: the humble ice pack).
My ice pack headband invention: patent pending
Another one you should switch your attention to immediately is Migraine Buddy. Download the Migraine Buddy app now. Go on, I’ll wait. I love this app. It allows me to keep track of the duration of an attack, the triggers, treatments, medication, symptoms, weather changes and sleeping patterns. It also allows me to post updates to social media informing my friends of my suffering with a handy screen cap tracking the hours as they climb up to 53 hour marathon sessions! A win win. Once you’ve clocked in a few episodes, you can start to see the patterns in the reports section. You can also send it to your doctor. Just don’t forget to update it when the migraine disappears, like that time I had a migraine for 6 weeks.
Now you have some solid evidence to back up your claims and give you more control. The next step is to find a GP that takes you seriously. My advice would be to ask in local communities, message boards or among friends for recommendations. r/migraine on Reddit is pretty great but not locally based. Otherwise you’re taking a huge risk in randomly turning up to a clinic and being assigned a doctor who will rush through a diagnosis, give you harmful medication or send you down the wrong path. Or worst of all, not take you seriously and make you feel like shit. We’ve all been there.
I eventually (and I can’t stress the ‘eventually’ here enough) found a great GP. She listened to everything I said, she addressed my concerns and needs. Even though she respected the treatment my neurologist had put me on, she inadvertently led me down an alternative and holistic approach by nudging me in a slightly different direction should I so choose to look elsewhere or find the medication not working. She put me on a chronic health plan with Medicare, a thing I didn’t know existed until she mentioned it. Basically if a GP refers you to a number of relevant specialists in psychology, physiotherapy, dieticians, etc. they can add it to the plan and you get a capped number of subsidised sessions through Medicare. Not only did she do this, she specifically recommended a physiotherapist in Leichhardt who specialises in headaches, and who she was sure could help me. Even though they had a physiotherapist in that specific clinic, she said it would be better to go to this specialist and almost insisted on it. I was so unaccustomed to this level of care and attention from a GP, I almost didn’t take her advice. I was extremely glad I eventually did.
Once it was clear that the amitriptyline was not only not working but making the migraines worse (and saw me gain 15 kilos in a few months, have severe nightmares, dry eyes and dry mouth) my neurologist told me to stop taking the medication and referred me to another neurologist who specialises in botox for migraine, since I was now in that category for treatment. I made an appointment and was told it would cost up to $500 for a first consult and then if I’m not eligible for the rebate, it would cost even more per treatment. Some people can justify this since botox is meant to be extremely effective in treating migraines. The problem for me wasn’t the cost. I’d spent so much money already over the years. The problem was that if it didn’t work, I would have felt like I’d exhausted all options and almost couldn’t deal with the emotional as well as physical ramifications. It was also only a short term solution in that it treats them, not prevents them. So before trying botox, I decided to give my last two alternative treatment options a red hot go.
Discovering Kate Mcleod the physiotherapist from The Physio Lab was a life changing turning point and I cannot recommend her enough. She asked all the right questions and was extremely thorough in listening to my back story. She knew about all the treatments I’d tried and why they hadn’t worked. She asked if I could hold off on the botox appointment to see if she could treat me first, because she was confident she could. She determined my body type — hypermobile — which put me at risk of migraines and headaches. She asked when the migraines got worse. Then she later asked when I started heavily using an iPhone and working long hours in an office and made the connection that modern life is a huge factor in exacerbating the issue, placing a huge strain on the body and specifically the neck. She predicts this will get worse for the next generation. She noticed even from the way I was sitting that I was susceptible to this. She even explained why having this body type makes you more susceptible to not only the adverse side effects I’d experienced on amitriptyline, but also that it makes you more prone to depression and anxiety. Light bulbs were going off all over the place.
Now here’s where it gets interesting. She explained how research has shown that the upper neck is connected to the brain, specifically to the sensitised brainstem, the cause of migraines. But many doctors and neurologists don’t recognise this connection. The medical world has long held the view that migraine is a vascular headache, related to the vasodilation of blood vessels within the head. But new research has shown that those suffering from migraines do not suffer from expansion of blood vessels in the brain, but rather from a sensitised brainstem.
This idea has been pioneered by Dean Watson. Dean Watson is the founder of the Watson Headache Approach, a form of treatment he’s taken around the world. Dean has been treating headache and migraine exclusively since 1991, amassing an extraordinary amount of experience with over 8000 headache and migraine sufferers. His approach is medication and radiation free, non invasive, and comprises a series of non manipulative (no ‘cracking’) techniques applied in a systematic way.
Dean Watson trained Kate, who referred me to Dean after a few sessions to get a comprehensive consultation and make sure she was on the right path. My session with Dean was one of the most illuminating healthcare sessions I’ve ever experienced. Prior to the session he called me to discuss my case and give me a heads up about what to expect in the appointment, how long it would take and what he would discuss with me. Once at the clinic, his wonderful wife Jane Watson made sure I was comfortable while I waited. Did I want something to drink? Did I know where the bathroom was? After the session she spent time talking to me about my experience and her own experience. I didn’t feel so alone and I couldn’t help but marvel at how different this felt to the usual experience of crowded waiting rooms and indifference.
During the one and a half hour session with Dean Watson, he patiently explained concepts, spent time asking me questions to assess my symptoms and condition, as well as lifestyle factors and treatments. He then showed me examples of the treatment, which included recreating the pain and then making it go away and demonstrating what had just happened via diagrams and videos. (“Now, let’s go to the movies!” Dean declared after the treatment, and I was fully prepared to grab my coat and actually go to the movies but he just meant to come and watch the video in slow motion that shows a 3D video of the brain and what he just did, which made a lot more sense now that I think about it).
The most groundbreaking thing about this has to be the revelation that for menstrual migraine sufferers, hormones aren’t actually to blame. This is a common misunderstanding that Dean clears up in this post where he explains that clinical observations show women experiencing headache not just around day 1 of their cycle (decreased oestrogen) but also at mid cycle/ovulation when there is increased estrogen. He also notes that hormones would affect both sides of the head equally, but menstrual migraine is often just on one side. Research has confirmed “that the hormonal profiles of women experiencing menstrual migraine are no different to those of women without menstrual migraine” so “how can it be hormones then?” Dean Watson rightly asks. This checks out in my case insofar as I’ve never been shown to have any problems with my hormones.
“This has prompted one of the world’s leading authorities in this area, Professor Elizabeth Loder, to suggest that there has to be another factor in the menstrual migraine condition; ‘… an abnormal response in the central nervous system to normal fluctuations of hormones.’ i.e. the issue lies within the central nervous system.”
This is where the sensitised brainstem comes into it again. Since hormonal changes trigger activity which is normal for most women — the subtle expansion and contraction of blood vessels with the head, this normal activity is exaggerated when it passes through a sensitised brainstem on the way to the cortex. The cortex, who is not having a bar of it now that it has received the exaggerated activity, interprets this as a harmful attack and it wants to warn the body of this, so it creates head pain (shakes fist at this huge misunderstanding on the part of the cortex). So in other words, as women we are supposed to experience a bit of pain from time to time, but it’s only when the brainstem is sensitised that this pain graduates into migraine territory.
I should point out that the Dean Watson treatment is not for everyone with migraines. There are specific things to look out for. The main thing is whether the migraine happens on one side of the head (it can be either side, interchangeably but most people experience it on the same side). The reason this type of sufferer might be struggling more than usual, is because it doesn’t matter if they change their lifestyle, their diet, their hormones, or go on the pill. The migraine triggers are still there and the root cause (the sensitised brainstem) hasn’t been addressed. This type of sufferer might say they’ve tried everything and nothing has worked. But they might find that prescription medication like triptans (ie. imigran) do work for them. That’s because imigran does desensitise the brainstem but only temporarily.
Still not sure of this theory? So my physio Kate gave it a whirl and she suspected the C3 cervical spine on right side to be the perpetrator (since the headaches mostly happened on the right hand side of my forehead). She pressed on it and it was the most painful thing I’ve ever experienced. She pressed the other side. Not so bad, but not great either. She said she applied the same amount of pressure to both. The one on the right one was stiff and out of place. She pressed on it for a while and eventually was able to recreate the migraine on my lower right hand side of the head, shooting up to the ear. She was also able to recreate the dizziness and nausea. I was horrified. And then she made it go away by relieving the pressure. This is a sign that the treatment can work.
So did it work?
I broke my own rule of only doing one treatment at a time to know what really did work, simply because I was at breaking point and couldn’t handle another few months of the excruciating agony of migraines. So I started the physiotherapy at the same time as I started acupuncture and taking traditional Chinese herbs. I was told with the Dean Watson approach, you only need up to five sessions to address the core problem and start to see results. I was told with Traditional Chinese Medicine I’d need two months before I see results.
I saw Kate sporadically at first and then more consistently and I was seeing results. But Kate did warn that I could still be susceptible to the problem if I didn’t pay attention to my working environment, making sure my desk was set up correctly (hot desking be damned!) and being aware of how my neck is when using the phone or a laptop, or even talking to someone from the side for too long, or if I did a strenuous yoga class or pilates without a trained physio present. She said some of the triggers could still set me off if enough of them happen at the same time and so there could be a few factors against me. I did have about 5 sessions with Kate and then one session with Dean, who recommended I continue seeing Kate as the problem was still there. But I didn’t go back to Kate for a while because…
The migraines went away. And the only thing I was doing in that time frame between seeing Dean and them disappearing was the acupuncture and the herbs. I began to pay more attention to this treatment for another reason. I started to notice my other symptoms that I’ve struggled with for a long time were also being treated. No more severe PMS for up to a week (I had an endometriosis diagnosis at 23). No more nausea, general headaches and insomnia.
So what gives there?
Let’s talk about Traditional Chinese Medicine and acupuncture
If you are a chronic migraine sufferer, you would have inevitably had someone throw the ol’ “have you tried acupuncture” at you line since, everyone is an expert remember? Firstly I would like to say, like a lot of recommended advice, there’s never just one thing that can help you. Doing acupuncture itself, without understanding the full picture of what’s going on with you, might not make enough of a difference to keep you going back, and something like acupuncture takes time to really work (like all things, but we do get impatient here in the migraine world). In some cases, it might even make it worse before it gets better. And that would deter you from giving it a complete go. Which would be a shame. If you’re going to do it, do it properly.
The TCM view of migraines and headaches is that the causes and symptoms of headaches can be so different, and so headaches should be diagnosed and treated according to individual conditions. They look at how the head is closely connected with other parts of the body, and what external or internal factors impede the flow of meridians, disturb nutrient supply to the head and block the head orifices. This understanding does acknowledge that there are many triggers or causes for headache which affect the frequency and severity from individual to individual.
“Chinese medicine recognises more than nine different imbalances which can cause migraine symptoms, whether it be a liver or gallbladder channel disharmony, a deficiency of Qi or blood, an upsurge of Yang to the channels in the head, or a combination. Because of this, acupuncture and herbal medicine treatment provides specific and targeted relief of active symptoms, and reconfigures the body to deal with the imbalance at its core, reducing the frequency and severity of migraines long term. Most treatments for migraine in the Chinese medicine clinic involve acupuncture and herbal medicine to ease migraine symptoms and correct the underlying imbalance. Each case is different, but in my clinical experience, an initial course of six to eight weekly sessions with thorough re-assessment at each visit is a reasonable starting point. Modern studies of the mechanism of acupuncture to address migraine have found needling stimulates morphine-like molecules which block pain receptors. Traditional understanding is that as well as pain relief, acupuncture and herbal medicine work deeper to regulate the hormonal and nervous systems, restore free flow of Qi and allow the body to self-regulate and heal.” - Dr Katie Molloy
My TCM doctor Dr Chen is a former oncologist (he still specialises in helping cancer patients). Each session he checks my pulse, looks at my tongue and asks me what symptoms I’m experiencing. He’ll ask if the symptoms are better or worse than usual or the same. Some sessions he might go into more details. Since he is a doctor trained in both systems, he might look at blood test results, ultrasounds or MRIs and sometimes find details that GPs or neurologists have missed. This is followed by an acupuncture session that varies each week depending on the symptoms and what he’ll be treating that week. So one week he’ll focus on the nausea and insomnia. Another week he focuses on my neck, which might include applying heat via a machine trained on the neck area. Once all the needles are in, you lie there in the dark for half an hour (usually longer — which is better but sometimes people are alarmed by this and I have heard one woman call out “Dr Chen, did you forget about me” I felt sorry for her, I thought she must have been new, because once you realise that you can be in there for up to an hour, YOU LEARN HOW TO STRATEGICALLY FALL ASLEEP, IT’S GREAT).
Sometimes the session involves keeping the needles in around my temples, in my ear, in my wrists or my feet for six days following the procedure. He then leaves me with a range of powerful herbs to take every day, he says they are flowers and one is called “peony”. You take 5 different types of 11 herbs three times a day, so that’s 165 herbs a day, every day. He changes the amounts each week depending on what issue needs to be addressed.
The differences I noticed after starting to take the herbs include actually noticing the pain in my neck (sometimes instead of in my head, sometimes in addition to it) which I never noticed before (and which might be why I never thought to see anyone about my neck). I started sleeping better. I noticed I had better digestion and was starting to lose the weight I’d gained on preventative drugs and the pill. I no longer had intense period pain or lower back pain before menstruation (still during but not as badly as before). Even post pill acne started to disappear! And eventually, the migraines had downgraded to general headaches. And if I watched my posture and did my physio-instructed retraction exercises, they disappeared altogether.
The last thing to go was, frustratingly, the nausea. Dean Watson once told me that nausea is the migraine of the gut and it’s possible to not have the head pain but to only feel it in the gut instead (this is why children complain of stomach issues a lot). So it was no surprise that I was only experiencing the nausea for a few weeks after the migraines had lessened. But I explained this to Dr Chen and he focussed on the nausea for weeks until it disappeared.
So now I can’t remember the last time I had a 3-day debilitating migraine bender. Or even a full 24 hours of one. Now I might get a bit of a headache, but it goes away fairly quickly. So something is changing. If I had to guess, I would say it was a combination of the Dean Watson approach with the Traditional Chinese Medicine and acupuncture sessions.
Taking control of your migraines
I could write 4000 words on the experience I had prior to this in trying to get my migraines cured. In fact, I did write them. And then I cut them out because they reminded me of an extremely traumatic time I didn’t want to revisit. But they serve as a powerful reminder that the health care system we put so much trust in has a lot to answer for when it comes to migraine treatment. What I will say is that I wish I had looked for alternative options sooner, rather than blindly trusting neurologists and GPs. Or that when I did try those options, that I had spent as much time trying them as the conventional and accepted approaches that were clearly not working and were only making me feel sicker in new ways.
As much as I wish I had done more research sooner, I also realize that I didn’t have the energy or the time to dedicate to my health, to seek out as many opinions and as much information as possible. It wasn’t until it became a pressing and debilitating problem that I sat up and said enough.
What I have learned is that you have to take control of your condition and trust your instincts. The longer you have suffered without answers, the harder it can be, and it will still involve time, patience and money, just to rule out options and find the thing that works for you. And even then there are no guarantees. But seeking out people who get it can be life rupturing. These were just two new ways I explored and it took less than 3 months to see a difference. There are actually more I never even tried but picked up along the way. Like the Cefaly headband (which makes you feel like Wonder Woman I’m told), daith piercing (permanent hipster acupuncture?!) and of course, botox, are also meant to be highly effective. But like so many other treatments, they mostly treat the symptoms in the short term.
There are more options out there than you are led to believe. But you’re not alone in your suffering and there are things you can do to get your life back. But the first and most important thing is this: tune out bad advice and become the best expert in your body and what works and doesn’t work for you. Seek help and find communities that understand your situation.
I cannot stress this enough: becoming an advocate for your own migraine care is essential.
This post originally appeared on the Beautiful Voyager Medium publication.
How to Talk to a Friend About Depression
This advice is geared toward Generation Z but can work for people of all ages. Zach Hargrove writes from experience about how best to approach friends you think might be experiencing depression.
People are very picky about places.
Start with humor.
We’ve all been in situations when we don’t want to tell about our feelings when our friends ask about it. It is not a great feeling to say “I’m good” when you’re not. That is especially the case for people who suffer from depression who can never tell you what’s wrong. It’s why, if you assume that your friend is in the dark place, you have to know how to appeal to them. And this is how to make them “walk” towards the sound of your voice, instead of ignoring it like everyone else’s.
Right Place, Right Time
You can’t start a conversation with a friend about their depression right at the mall, bus stop or some birthday party. It would be the same as making a marriage proposal in the public bathroom with a ring made of gum that you’ve picked up from the floor. Even if your significant other loves you with all heart and wants to marry you, a big part of that person will not want to accept your proposal if you do it this way because of inappropriate atmosphere of that place. People are very picky about places. And when the topic of conversation is dedicated to their deep, personal feelings – the depressed ones take the cake. Waiting out for a perfect moment is not an option (for obvious reasons). That’s why you should properly initiate and create this moment yourself, if circumstances are against you.
The Wrong Way to Approach a Depressive Friend
1. Hey, you look sad
2. Let’s go out somewhere
3. I want to talk
Your Friend Will Think
1. I look sad because I am sad, you Sherlock
2. I don’t want to go anywhere
3. I don’t want to talk
This method is ineffective because of its lack of originality. For instance, most people would choose a wooden transformer instead of one of the zillion copies of green toy soldiers. Especially when they got used to receiving these toys almost every day and they don’t want to play with them. So, it is good idea to present something unusual.
The Right Way to Approach a Depressive Friend with Humor
1. You look sad. I don’t love you when you’re sad
2. Yeah, I’m not in the great mood as well
3. Let’s get some ice-cream or whatever you enjoyed eating in the past the most.
4. I need someone to talk to, Billly! Please, help me out.
Your Friend Will Think
1. He doesn’t love me when I’m sad? That sounded weird. Does he wanted to tell that he loves me only when I’m happy? What the hell?
2. Oh, you think you’re the one who’s in the bad mood! But I guess now we have a common topic to talk about...
3. I don’t like ice-cream… but I could go for some tacos.
4. Wow, he’s not having discomfort in asking for help. I’d say he’s even desperate to a certain degree. He’s my friend. Maybe it’s not a bad idea to go out, afterall. I might want to tell him something that’s bothering me if he asks.
IMPORTANT: Before we go any further, note that the following tips are useful only if your friend is not up to something important, like planned meeting, a test or an interview. If your friend is always available for a private conversation, scroll to the final paragraph of the article.
How to Use Humor With a Depressive Friend
One of the greatest ways of making it difficult for person to refuse your any proposal is to apply a good sense of humor. Humor is a tremendous tool for taking any person into a talking zone. And even if your friend experiences a high level of sadness and has no desire to laugh, you can still force him to smile sincerely within a minute if not couple of seconds. A good way of starting doing that (if there are no humorous inspirations around) is to go to the inside jokes. This method of making someone smile will be a reminded of that you are one of the very few people who can identify with that person in this peculiar way. That is why you will be appreciated and will be more likely to receive a positive reaction.
2 Easy Ways to Make Someone Laugh
1. Play Tommy Wiseau’s “You are tearing me apart” scene from “The Room”. It’s okay to refer to your friend as Lisa. If your lines didn’t work, say “take 2… action!” slap your hands and play the scene again.
2. Threaten to bite if you don’t go out for ice-cream together. It is important to stay this phrase dead serious in order to make it sound and look hilarious.
Many people will disagree with this method at first. They will state that it is overly aggressive and provocative. Because it is. When we talk about friendship, we have to understand that the real friends sometimes have to be rude to each other. It’s like with the people who suffer from an alcohol addiction and don’t see the problem. They need someone who can cynically tell them what’s wrong. Otherwise, that person won’t see how it effects you and your friendship.
Another good point in support of this move is the fact that people love drama. And depressive people are the most passionate about it. That is why if you give them this bit of dramatic nourishment, they might want to give you what you want in return. The following examples will help you to get the idea how to do it properly.
Right way: “Go fuck yourself! You are the only friend I want to talk about my problems. I’m trying my best to make you laugh so that you could get in the nice mood and agree to go out for some free, delicious ice-cream and all I hear is “no”. If you don’t want to help out your friend simply by listening and eating, then you’re fucking asshole!”
Your anger can actually make your friend chuckle or even burst into laughter. Of course, If that person cares about your friendship, there’s also a possibility that he will feel guilty at the same time. That way, chances of him agreeing to go out will increase.
If you played the victim perfectly, and your friend still refuses to go, you have to deliver the following message:
“Look, you are my friend and I care about you. I don’t want to fight with you over my problems. I’ll try to handle it myself. I’ll be in touch”
Remember, that it is important to walk away with making sure that your statement was interpreted correctly.
The Proper Way of Asking
Before even starting a conversation with your friend, think of yourself as a professional interviewer. Generally speaking there are two types of interviewers: straightforward knuckleheads and patient, mental picklocking specialists. The first group of journalists almost never succeeds in getting full information from the person they interview. They might get an expressive reaction followed by strong desire to end the conversation. But that is not what we want from our friend who is having some issues. What we want is to use tactics of a legit interviewer. The one who will apply a surgical attitude and extreme carefulness in ability to unnoticeably pull the necessary thoughts out from the head of his guest. Sounds like some manipulation? Because it is! But lord knows that you are using this mental scalpel for good. So in order for this surgery to go on well – take your time.
Don’t
1. Start by assuming your friend suffers from depression
2. Then say, “I’m starting to worry about you “
3. “What’s wrong?”
As it was mentioned earlier, depressed people like to overdramatize. Thus, if you go to the “wrong way” strategy, they will likely think..”So he was lying to me. It was a white lie, but still… you all people lie!” or “It will take forever for me to explain what’s wrong.” “He won’t understand my problems” or “Do I go for “I’m good” option this time?”
Most people are not open about their feelings when they’re having problems. That is why it is better to use another option, that involves you taking your time.
Instead…
1. If I was a typical parent who suspected that his son smokes, I’d say something like this:
“Brian, for the third time in this week I sense the smell of cigars on your clothes. I’ve just seen a round burn on your wrist. I believe you have something to say to me”
2. But I am your friend. And I suspect that you’re having a tough times. And that is why I have a bit different speech:
“Brian, for the third time in this week I notice that you look unhappy. I don’t want to bother you, but I also want to know what’s going on. I know it can be difficult to open up about it. But since I am your friend, let me look through the peephole with this simple question. What is one of the things that bothers you the least lately?
You have to go from general questions to more detailed and personal. It should be the same as putting someone in a warm bath, instead of throwing person into the hot one. All you have to do is gradually increase the temperature to the one that your “bathing subject” will be okay with. So be conscious, and you won’t boil your friend.
This whole strategy will make your friend appreciate that you didn’t make the situation awkward by being straightforward like most people if not everyone. But even if he won’t notice it, it will create a comfort. That will lead to good chances to tell you what is the problem.
P. S. There’s also a good chance that you are the one who suffers from depression and feels uncomfortable to start to talk about it. If that’s the case, you can always send this article to someone whose support you’d like to have and ask that person to scroll it down till the end.
About the author
Zack Hargrove is a freelance editor and writer. Most of his topics are dedicated to music, education and ways of strengthening your scientific curiosity. He notes, “I originally wrote this for a college class, but my professor refused to accept my paper because there is cursing in the piece. I wanted to share it as a guide because these are the tips that still help me to find out a lot about people I care about.”
My Unhealthy Mental Habits and How I Changed Them
Written by Texas-born singer/songwriter Jon Pattie, this post provides insight into how one person tackled his own unhealthy mental habits to help you do the same.
The author with his very nice, well-intentioned parents.
Living on your own for the first time is a difficult transition for anybody. Your parents, God bless them, try to prepare you as well as they can for the real world. My parents did a great job. They taught me how to be studious. They taught me the importance of healthy eating and budgeting. They taught me honesty. But one thing they never had the opportunity to show me was how to properly handle my own emotions. How to handle anger, sadness, and frustration was an enigma to me. I’ve used music and songwriting throughout the majority of my life to help but that can only go so far. You can’t leave in the middle of a disagreement to go write a song about how pissed off you are at the other person!
The author in the studio. “Songwriting helps,” he says, “but it can only go so far.”
“I didn’t fully connect with this book,” says the author, “but it did ignite my curiosity.”
The best, and worst, part of living on your own is it helps show you what habits you have in your life. Whether they be good habits, like waking up early to go to the gym or making study time every evening, or bad habits, like finishing a 12-pack alone when you’re feeling overwhelmed or using negative internal dialogue in your everyday life. Habits can make or break a person, make or break a career, and make or break someone’s dreams and aspirations. This past year I have been studying the power of habits and the one consistency I’ve noticed is nearly every major success story surrounding an individual was built off of a strong foundation of healthy habits!
The best lesson I’ve learned through my journey of bettering my habits is that it only takes one small step to start. The first step I took was picking up a self-improvement book about Ayurveda. Although that first book didn’t connect with me as well as it could have, it ignited my curiosity. What other self-improvement books are out there? What other unhealthy aspects of my life have I been ignoring?
The author with his friend and mentor, D Grant Smith (on the right).
This curiosity into bettering myself only grew when I began working with my now friend and mentor, D Grant Smith. On a whim, I decided to take a session with D who works as a life coach for personal development. One conversation later and I knew I had some work to do. After our first talk, D instructed me to begin a new daily ritual: affirmations. Immediately upon waking up and right before bed, I was supposed to read my list of ‘affirmations’. Honestly, the first time he pitched this idea to me, I disregarded it mentally. “Isn’t that what losers do? Tell themselves they are awesome and great? Why would I need to tell myself that? Shouldn’t I just know it?” I know. That’s some pretty ass-backwards logic.
But after thinking about it, what did I know? Here I was, 23 years old, I hated myself and I hated the choices I made on a daily basis. Why not try something new, even if I did think it was crazy mumbo jumbo? So once again, I took a first step into a new habit.
Picking up the habit of daily affirmations was a bit rocky at first. I really only did it once a day every now and again. But I kept at it. Thankfully I had the support of those around me to stick to these new habits. Even though it took a few weeks, I eventually was saying my affirmations once or twice a day probably five days a week. It had reached the point to where I was now thinking of these affirmations during my normal workday. And I wasn’t just saying these affirmations, but I was believing them too. I was living them. I am confident. I am passionate. I am great!
And all of this began because I took one small step. I picked up a book two years ago. Then I took another small step, I had a consultation with a life coach. Then step-by-step I started my journey to becoming a better person. Now, I write my affirmations every morning and evening in my journal where I also write my goals for each day, and my gratitude list. This is just a small part of the habits I’ve been able to use to improve my life but it all started with just. One. Step.
Texas born singer-songwriter Jon Pattie’s passion for songwriting was clear from an early age. “Pattie’s soul-shattering vocals have the power to provoke a profound response,” says fans.
Pattie is currently preparing a four-part EP project that will take his artistic development to the next level. Each album will recount a new portion of Pattie’s journey about his search for who he is and the man he wants to be. The first album, Reflections Volume 1, released on November 7th, 2018.
Follow Jon Pattie: Facebook I Twitter I Instagram I YouTube I Spotify